中国组织工程研究 ›› 2018, Vol. 22 ›› Issue (7): 997-1002.doi: 10.3969/j.issn.2095-4344.0108
• 人工假体 artificial prosthesis • 上一篇 下一篇
直接前侧入路与后外侧常规入路微创全髋关节置换的稳定性比较
高 益,瞿玉兴,周 祺,王 斌,郑 冲,罗立立
- 南京中医药大学附属常州市中医医院骨一科,江苏省常州市 213000
Comparison of the stability of direct anterior approach versus posterolateral approach in minimally invasive total hip arthroplasty
Gao Yi, Qu Yu-xing, Zhou Qi, Wang Bin, Zheng Chong, Luo Li-li
- First Department of Orthopedics, Changzhou City Hospital of Traditional Chinese Medicine Affiliated to Nanjing University of Traditional Chinese Medicine, Changzhou 213000, Jiangsu Province, China
摘要:
文章快速阅读:
.jpg)
文题释义:
微创全髋关节置换:已经逐渐发展为两大类,一类是仅仅在传统全髋关节置换的基础上缩小皮肤切口,而皮下组织分离、切除与传统的全髋关节置换一致,且该手术切口与坐骨神经邻近,术中容易导致坐骨神经损伤,该类手术中最为经典的为Gibson入路、Hardinge入路等,这并不是完全微创。另一类则是在新的解剖位置微创入路,此入路强调从肌肉间隙进入,不破坏外旋短肌和臀中肌,因此从软组织保护的角度讲,这才符合真正的微创要求,其中以直接前侧入路最为经典。
直接前侧入路:为Smith-Petersen入路的一种改良术,与Smith-Petersen入路相比直接前侧入路切口更靠外侧,从阔筋膜张肌、缝匠肌和股直肌之间的解剖间隙(Hueter间隙)穿过,不切断髋关节周围肌肉组织,从而真正实现在神经血管和肌间界面操作手术。该方法因具有术后出血量较少、组织损伤较轻、术后恢复快、下床活动早、并发症较少等优点,近年来在国外得到广泛应用。但是该手术入路操作困难,学习曲线比较长,不过随着术者经验的增加,术中并发症的发生率会逐渐降低,而且随着手术技术的提升与手术时间缩短,直接前侧入路手术的输血量、失血量均有减少趋势。
摘要
背景:目前微创全髋关节置换逐渐发展并成为全髋关节置换的代表性术式之一,而直接前侧入路具有组织损伤小、术后并发症较低、术后恢复快等优点,但是与其他入路相比较而言,该入路是否可获取更优的早期、远期疗效还存在较大争议。
目的:对比直接前侧入路与后外侧常规入路微创全髋关节置换的临床疗效。
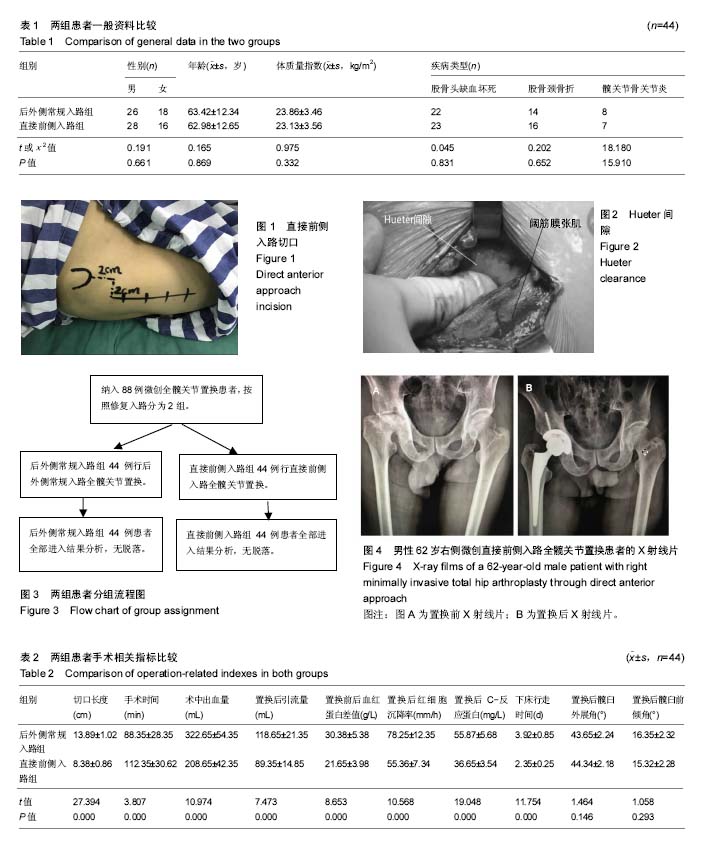
方法:选择2015年9月至2016年9月于南京中医药大学附属常州市中医医院骨一科行微创全髋关节置换的患者88例,按照修复入路将其分为后外侧常规入路组及直接前侧入路组,每组44例。记录并比较2组患者手术切口长度、手术时间、置换后引流量、输血量、置换前后血红蛋白差值、下床行走时间,术后髋臼外展角和髋臼前倾角,置换后红细胞沉降率和C-反应蛋白水平,并发症(感染、血管损伤、髋关节脱位等),以及术前、术后1,3,6个月的髋关节功能Harris评分等。
结果与结论:①2组患者术后髋臼外展角和髋臼前倾角差异无显著性意义(P > 0.05);②直接前侧入路组患者的手术时间明显长于后外侧常规入路组(P < 0.05);而直接前侧入路组患者的手术切口长度、术中出血量、置换后引流量、血红蛋白差值、置换后红细胞沉降率、置换后C-反应蛋白以及下床行走时间均明显小于后外侧常规入路组(P < 0.05);③直接前侧入路组患者置换后1,3个月Harris评分明显高于后外侧常规入路组(P < 0.05);2组患者置换前和置换后6个月的Harris评分差异均无显著性意义(P > 0.05);④2组患者在置换后并发症方面差异无显著性意义(P > 0.05);⑤结果提示,后外侧常规入路和直接前侧入路微创全髋关节置换的随访6个月疗效和置换后并发症发生率无明显差异;但直接前侧入路手术创伤更小,患者术后恢复更快,关节稳定性更高,更符合微创手术和快速康复理念的要求。
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
ORCID: 0000-0003-2501-1542(高益)
中图分类号:

.jpg)